News & Events
Stay up to date with all the latest news and events from C4 and the broader cervical cancer control field.

Major Australian Government funding boost to eliminate cervical cancer in our region
Australia is stepping up its regional leadership in the elimination of cervical cancer, with the announcement today of a $12.5 million Australian Government grant to a consortium of leading Australian and

Australia takes ‘EPICC’ step towards fairer cervical cancer outcomes in region
Australia is stepping up its global leadership in the elimination of cervical cancer, with the announcement today of a $12.5 million Australian Government regional aid grant to a nongovernment consortium headed by the

National Strategy for the Elimination of Cervical Cancer in Australia and our region
The C4 is thrilled about the announcement today by the Australian Government of the release of the National Strategy for the Elimination of Cervical Cancer and a $48.2 million investment

Congratulations to all those involved in a successful virtual Eliminating Cervical Cancer 2023 (ECC2023) Conference!
On Friday 17th November, Cervical Cancer Elimination Day of Action 2023, the C4 hosted the first ECC2023 (previously named the Preventing Cervical Cancer Conference [PCC]). The theme of the conference
The Compass Trial: Recognised as One of the Most Important Clinical Trials in 2023
Nature Medicine recently published an article featuring the “11 Clinical trials that will shape medicine in 2023”, which listed the top clinical trials to watch over the course of the year
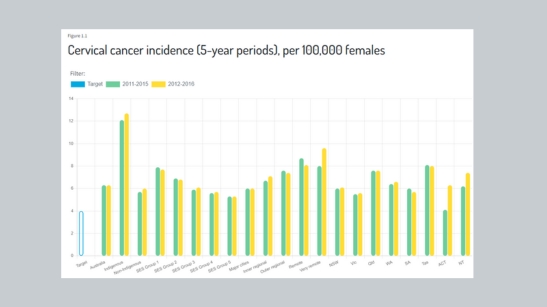
Release of the 2022 Cervical Cancer Elimination Progress Report
In this second data audit of Australia’s progress towards the elimination of cervical cancer as a public health problem, we have brought together the most recent data available across 12